Exposure to discrimination also affects patient’s health outcomes and contributes to health inequity. Structural racism and bias can negatively affect a person’s access to health care, as well as many circumstances that contribute to their wellbeing, often referred to as social determinants of health.
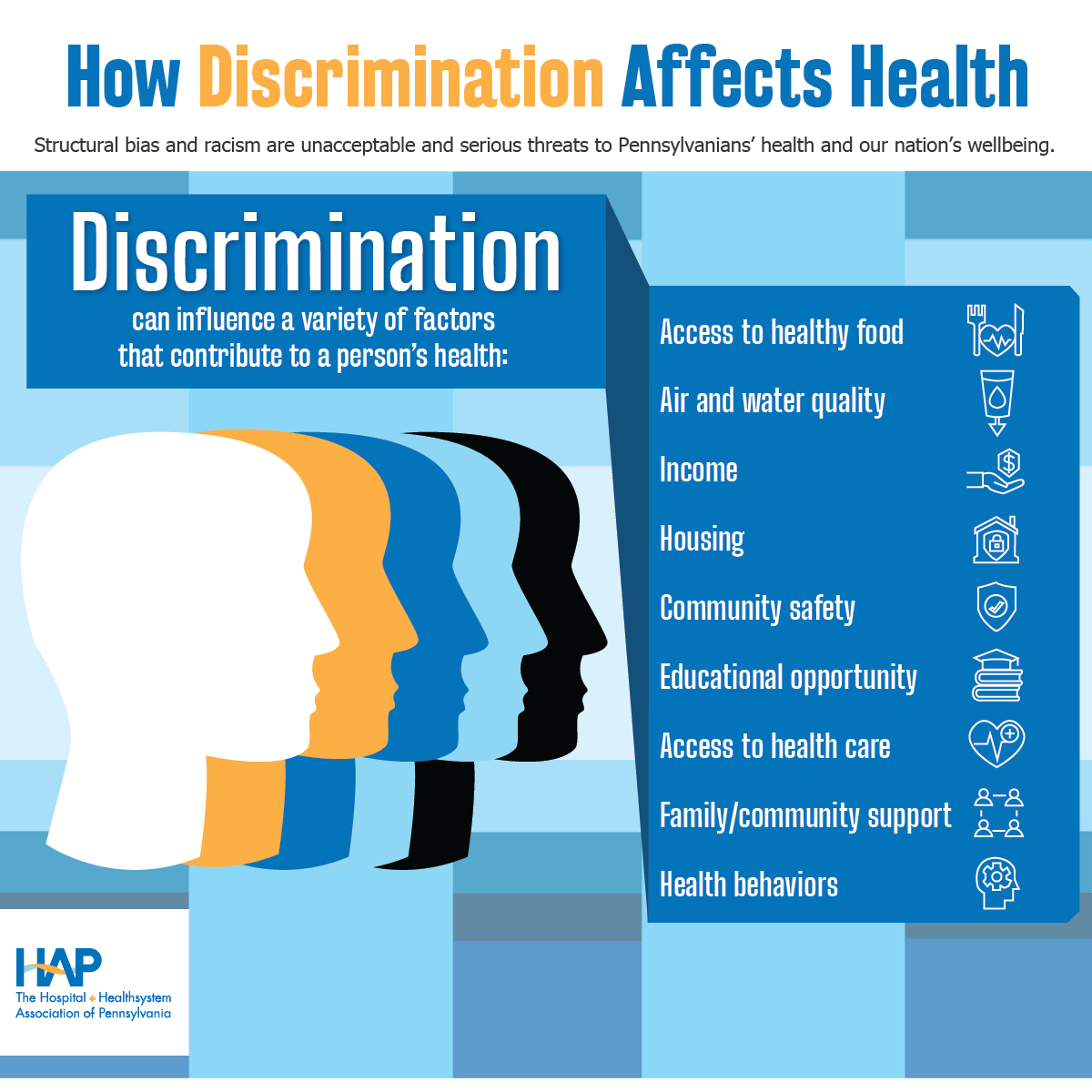
For example, discriminatory housing practices and public policies have resulted in communities of color being disproportionately affected by factors such as unhealthy air or limited access to healthy food. Discrimination against LGBTQ communities has resulted in higher rates of homelessness. All these factors affect a person’s health.
Health care providers and organizations can address patients’ exposure to discrimination by understanding the health effects of discrimination and working to counter them through the care they provide and community advocacy.
Achieving health equity requires addressing BOTH provider bias and patients’ exposure to discrimination.